My Cancer Diagnosis and Updated Outlook
biography My Cancer Diagnosis
Well now, it’s been 2 years since my last post. The kids have gotten a lot bigger but not much else has changed. My last company, TenSixteen Bio declared bankruptcy and I left a week before the official layoffs so naturally, I missed a few months of severance. However, I landed on my feet and started a new job at Precede Biosciences in the fall of 2023.
So what does the company do? Well, I figured now’s a good time to show off some of these new LLM AI capabilities the world is going crazy over, but still struggling to find applications for. Case in point, I am using the Cursor IDE to write this post (disclosure: I also use it for work and have a real license) and the AI is trying to write the post for me… despite having no context about my life!
“ChatGPT, tell me about Precede Biosciences but provide your output in jekyll kramdown markdown block quote format so I can copy paste it into my post”
Precede Biosciences is pioneering advancements in precision medicine by developing a first-in-class liquid biopsy platform that provides unprecedented insights into disease-defining biology from a simple blood test. PRECEDE.BIO
Their innovative platform profiles circulating chromatin and the DNA methylome from just 1 mL of plasma, offering genome-wide resolution into the dynamic activation of individual genes and pathways. This approach enables the detection of actionable, transcriptionally regulated drug targets and resistance phenotypes, facilitating more precise therapeutic decision-making. FINANCE.YAHOO.COM
By partnering with drug developers and academic researchers, Precede aims to improve success rates in drug development and create a future where every patient can receive a rapid, minimally invasive diagnosis and therapy tailored to the biology of their disease. PRECEDE.BIO
See? Easy peasy!
Bloody stools!
This story begins with bloody stools. I can’t recall when I first began observing them but it was probably around late 2023. The wipe came away red and I was frankly quite terrified. However, having never dealt with this before, I decided to wait and see if it would occur again. About a month later, it did, and then the frequency became weekly. Eventually, the stools themselves would have small blood clots and additional mucus. At this point, it was March 2024 and I was scheduled to see my primary care doctor for a routine checkup. I noted the issue and my doctor referred me to a GI doctor.
My primary care doctor is part of the Beth Israel Deaconess Health System and I was referred to a GI doctor at their main campus in Boston, however, the appointment wasn’t until October 2024! Granted, it was partially my own fault for delays in making the appointment but it was still 3 months out from my initial call.I was hopeful it would be something benign.
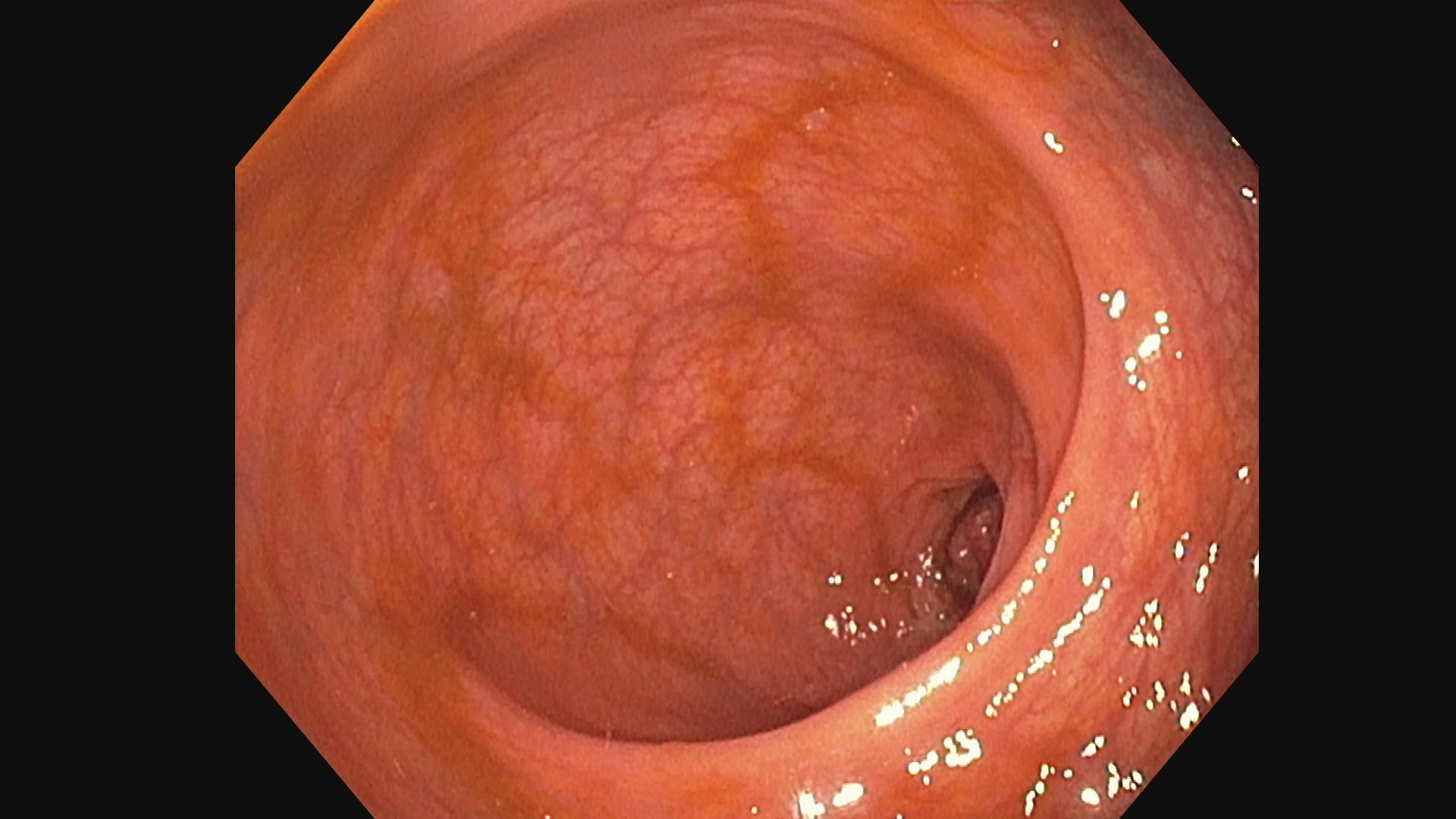
When the day arrived, I discussed my observations and symptoms with the doctor and he ordered a colonoscopy. I wasn’t particularly excited about my first colonoscopy but decided it was better to be safe and get it over with. I was hoping for a best case scenario and while aware of the worst case scenario, I didn’t dwell on it much.
The colonoscopy
For those of you who don’t know, a colonoscopy is a procedure where a doctor inserts a camera into your rectum and then into your colon to examine the inside. It’s a bit uncomfortable but not particularly painful. To prepare for it, you do something called “bowel prep” which involves consuming copious amounts of a laxative solution, then shitting your guts out for 24 hours. It’s a very inelegant cleanse type process.
My bowel prep involved drinking a disgusting solution called SuPrep. It’s basically a thick, sugary, and salty concoction; you chug it down and in less than an hour, the shits start. The day of my colonoscopy, I was basically pooping water the color of mountain dew.
For the colonoscopy, they gave me an IV and actually brought a anesthesiologist in to sedate me. They gave me propafol and I took a wonderful nap. When I awoke, I was groggy and felt refreshed but the piece of paper they handed me left me concerned.
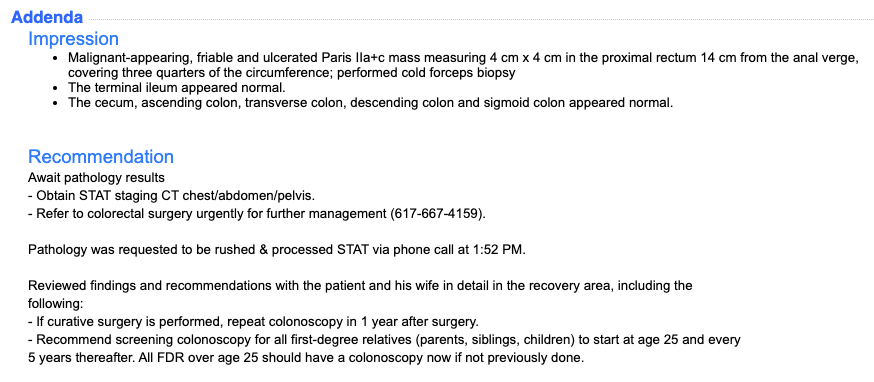
- Malignant-appearing, friable and ulcerated Paris IIa+c mass measuring 4 cm x 4 cm in the proximal rectum 14 cm from the anal verge, covering three quarters of the circumference; performed cold forceps biopsy
- The terminal ileum appeared normal.
- The cecum, ascending colon, transverse colon, descending colon and sigmoid colon appeared normal.
The pathology report
At this point, I was mostly grappling with my new reality. I googled the words from the initial impression and none of it was good. There was nothing more for me to do so I painfully waited through the weekend for the pathology report.
I should note that the period of time between the colonoscopy results and the staging were the most challenging. My mind was racing and trying to process the implications of the diagnosis but I was also in a complete information void. Working adjacent to oncology my whole life, I was well aware of the spectrum of outcomes so not knowing where I landed on that spectrum was particularly difficult. Sleep was hard to come by and my waking moments were filled with thoughts of my own mortality, and what effect this would have on my family. Needless to say, I had lost my appetite for weight as well as the things I normally enjoyed. I still had no idea how or when to break the news to my family and friends but I was certain they would be supportive and that gave me some comfort.
Eventually, the pathology report came in.
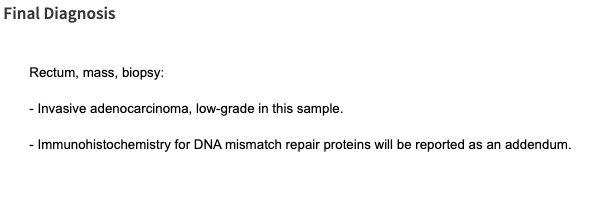
Healthy tissue.
Cancerous tissue

Staging
The next step is staging. For the uninitiated, cancer is roughly broken into 4 stages: stage I - IV. I won’t get into the details but maybe ChatGPT can give me a blurb about cancer stages.
Cancer staging is a standardized way to describe the size, extent, and spread of cancer within the body. It helps doctors plan treatment, estimate prognosis, and facilitate research. The most commonly used system is the TNM staging system, developed by the American Joint Committee on Cancer (AJCC) and the Union for International Cancer Control (UICC).
TNM Staging System
- T (Tumor): Describes the size and extent of the primary tumor (T1-T4, with T4 being the largest or most invasive).
- N (Nodes): Indicates whether cancer has spread to nearby lymph nodes (N0-N3, with higher numbers indicating more node involvement).
- M (Metastasis): Determines whether the cancer has spread to distant parts of the body (M0 = no spread, M1 = metastasis present).
Stage Grouping (0-IV)
The TNM components are combined into an overall stage:
- Stage 0: Cancer is localized to the top layer of cells (in situ) and hasn’t spread.
- Stage I: Small tumor, localized, and has not spread to lymph nodes or distant sites.
- Stage II-III: Larger tumors with increasing local spread to nearby tissues or lymph nodes.
- Stage IV: Cancer has spread to distant organs (metastatic cancer).
Cancer staging helps guide treatment decisions, from surgery and radiation in early stages to systemic therapies (like chemotherapy and immunotherapy) for advanced stages.
Thanks ChatGPT. Now that we got that out of the way, it will be a lot easier to describe the results of my staging. I did a contract enhanced CT scan and MRI with BIDMC. The collective imaging were assessed by a radiologist and the BIDMC team called it a T3N1M0 tumor. This puts me at early stage 3 with one lymph node involved and no distant spread. However, when I met with the oncologist and surgeon following their tumor board review, they noted that the lymph node was questionable.
Based on the staging, and citing the recent PROSPECT study, the recommended treatment plan was to do 6 cycles of FOLFOX chemotherapy, followed by a low anterior resection surgery to remove the tumor, adjacent lymph nodes, and some margin, then follow it up with 6 more cycles of FOLFOX. Quite the treatment plan, and definitely no walk in the park. At this point, I was mentally preparing myself for the difficult road ahead but I began to feel more hopeful as the disease was localized and I wasn’t staring down the barrel of a stage 4 diagnosis, which has much lower 5-year survival rates and outcomes.
A second opinion
I shared the news with my family and my sister suggested I get a second opinion from Dana-Farber Cancer Institute (DFIC) and Brigham Women’s Hospital (BWH). The Boston area is world famous for their medical care facilities and practitioners so I knew I was in good hands either way but I figured the second opinion couldn’t hurt.
I had my scans and biopsy slides sent to and reviewed by the DFCI and BWH teams. They met with their pathologists, radiologists, and tumor board and arrived a slightly different conclusion. Their call was that the tumor was T2N0M0 which would be stage 2 and offered a different treatment plan.
They recommended that I forego the neoadjuvant chemotherapy (pre-surgery) and just go straight to the surgery, then based on the pathology analysis of the resected tissue, they would determine the appropriate course of action.
I am so very very grateful that I got the second opinion as the new treatment plan could spare me the initial 6 cycles of FOLFOX and I would get to remove the tumor immediately. This whole time, I had an unsettling feeling that my body was trying to kill me. It’s a strange feeling and I was overwhelmed with reactionary anxiety, wondering what decisions I made that led me to this point. What combination of bad habits, diet, lifestyle, and genetics led me here?
Those thoughts were never constructive and having an actionable plan ahead of me, I was able to better put those thoughts to rest. At the time of diagnosis, I weighed about 185 lbs. By the time of my surgery, I was already down to about 175 lbs. Having already made several lifestyle changes for the better, I was determined to come out of this ordeal stronger and healthier than before.
The surgery
The surgery was scheduled for December 6th, 2024, a Friday. Prior to the surgery, the surgeon did a flexible sigmoidoscopy to get a better look at the tumor and the surrounding tissue, as well as tattoo the tumor so it would be visible from the outside during surgery.
The surgery was a laparoscopic low anterior resection. It is minimally invasive and they make 3 small incisions where they insert the camera and instruments. They pump CO2 into my abdominal cavity to inflate it and create a working space, then cut out the tumor and lymph nodes. Once that’s done, they staple the two ends together to form an anastomosis.
I was spared a colostomy bag since I had no prior radiation or chemo. When I awoke from the surgery, I had two IVs, one in each hand, and a Foley catheter in the penis. As the meds wore off and the pain set in, I was surprised to find that the discomfort from the Foley catheter was the worst part of it.
The first night post-surgery, I was given plenty of pain meds and I was quite hungry having not eaten the previous 48 hours. All they gave me were ritz crackers though, at least until I was able to fart and poop. That was a big hurdle for me to clear and I was able to do it the first night. That first fart was amazing but due to my muscle weakness following the surgery, I was basically lacked all lower and mid abdominal muscle usage and you would not believe how much you use those muscles for everything until you can’t use them.
That first night, I farted, shat myself, and ate ritz crackers. I was unable to sleep since the nursing staff kept waking me up to take vitals, or waking up my roommate to get his vitals.
The next day, I was determined to get the Foley catheter out. I pleaded with my nurse, Lucy, and am so thankful she advocated for me. She was able to get one of the doctors to come speak with me about why the cathete was still needed and what the risks were in removing it now. Basically, the surgery takes place in a location that has a lot of sensitive nerves involved the bladder emptying process. If there was any damage at all, I could be in a state where I am unable to empty my bladder on my own, hence the catheter. Usually the cather is removed after 2-3 days, but I was really suffering and couldn’t imagine another night with this thing in me. So I acknowledged the risk… basically if they take the catheter out and I can’t pee on my own for 8 hours, they’re gonna put it back in, and that would REALLY suck.
So Lucy got the go-ahead to pull the thing out and damn did it suck. Very painful but the relief was immediate. I then started pounding water and within 2 hours, was able to pee on my own. Though there was a significant burning sensation, that was likely due to the catheter irritating the sensitive lining of my urethra.
The same day, I was able to eat whatever I wanted so I started with some scrambled eggs and toast. I also started walking as that is supposed to help with the recovery process.
By the next day (Sunday), I was sick of the hospital and just wanted to rest in my own home. My folks had flown in to help out and I had met all their criteria for discharge and so, by day 2 post-surgery, I was on my way home with a bag of oxy and lovanox. Lovanox is an anti-coagulant that I needed to inject subcutaneously once a day for the next few days / weeks to prevent blood clots. Walking also helps prevent blood clots. Even though the Lovanox needle is small, I still hated jabbing myself every day.
The recovery
The first week was rough. Not being able to exert any force while pooping meant waiting for the poop to come out naturally with gravity’s assistance. Luckily, my digestive track was still working itself out so all my poop was soft and fluffy. It looked like little brown clouds floating in my toilet water. By the second week, the pain was much more manageable and I was eating more. I still avoided large meals as distending my abdomen was very painful for the muscles that were still healing.
By the end of the second week, I had a check-in with the surgeon and oncologist. I was healing up nicely and other than a small hematoma above the incision, I was doing well. The results of the resected tissue analysis were in and the margins were clear, the lymph nodes were clear, but the tumor had breached the outer layer.
The final staging was T3N0M0.
I was ecstatic about these results, I was essentially cancer free (undetectable at least) but the oncologist recommended I do 8 cycles of FOLFOX to squash any micrometastases and improve the likelihood I remain cancer free for the next 5 years.
The chemo
Prior to chemo, I would need a port installed. The port is basically a long-term IV which sits under the skin on my chest and has a catheter which enters the vein in my neck and hangs down into the vena cava. It basically gives direct IV access to a large vein which goes right into the heart for distribution of the chemo.
The surgery was very minor with no full anesthesia, just a little lidocaine, fentanyl, and other drugs to keep me comfortable. The recovery was weirdly long though, for the next two weeks, I felt discomfort when swallowing from the incision on my neck, and I was very aware of the thing that was now under my skin on my chest.
Of course, I didn’t have long to recover as 3 days post surgery, I was slated to start my first cycle of chemo.
Having never done chemo before, I was nervous but also interested to learn about how it would all work. So here’s how it goes, the cycle is two weeks long, on the first day, they draw blood and run labs to check blood cell and platelet counts, as well as kidney and liver function. They draw these labs through the port that was installed. Then I meet with the Oncologist and discuss the previous cycle, any side effects, how I’m feeling, etc… Then the infusion begins. They give me pre-meds to mitigate nausea and any other effects that might occur once the infusion starts. Then they connect my port to the chemo pump and for 2 hours, I get infused with Oxaliplatin and Leucovorin.
After the 2 hour infusion, they give me a bolus of 5-FU then send me home with a pump to infuse more 5-FU at home over the next 46 hours. The pump is pretty annoying to have but it’s not too cumbersome.
On day 3, I get to manually disconnect the pump, flush the IV, and pull the needle out of my chest. My previous work in cell product manufacturing has familiarized with me the components and connectors involved so this part was pretty easy.
Day 4 is the worst in terms of side effects. The steroids and other pre-meds have worn off so my energy tanks, I get a little nauseous, constipated, and have no appetite. I basically just sleep all day.
Day 5 gets better and each subsequent day I begin to feel more normal. By the second week, the recovery week, I basically feel completely normal but as the next cycle approaches, I definitely feel a sense of impending dread.
The main side effect I’ve noted is peripheral neuropathy. A tingling pins and needles sensation in my hands when they get cold and a shock when I touch something cold. Drinking cold water is torture and feels like I’m swalling broken glass.
Where I am today
Today, I have completed 3 cycles with 5 more to go. Overall, I am maintaining a positive outlook. It has crushed my social calendar as I’ve basically been isolating since I started but my friends have been very supportive and delivering food to me on occasion. My wonderful wife has taken time off work with FMLA and has taken on all responsibilities for the kids’ schedule, as well as doing all the things I am not able to do.
I want to thank my friends and family for their support. I also want to thank Dr. Irani at BWH for the surgery. Executed to perfection with no complications and a smooth recovery. A special thanks to the nurses at BWH, especially Lucy who advocated for getting the Foley catheter out, greatly improving my quality of life. Thanks to Dr. Huffman at DFCI for the chemo plan and the entire team at DFCI for their expertise and care. Honeslty, there was such a massive mobilization of resources and coordination of care that I almost feel undeserving of the effort. Everyone who played a part in my care, no matter how big or small, thank you.
It’s crazy to think that for me, that surgery was a huge life-changing event, but for Dr. Irani, it was just another day at the office, saving lives.
I am really looking forward to being done with chemo and when I am done, I either want to get a dog or trade-in my Golf for a sports car, maybe a C6 or C7 Corvette?


